Decoding Transaminitis: Your Comprehensive Guide to ICD-10 Codes
Are you searching for clarity on the transaminitis ICD 10 code? This comprehensive guide provides an in-depth exploration of transaminitis, its diagnostic coding under the International Classification of Diseases, Tenth Revision (ICD-10), and everything you need to know for accurate medical billing, data analysis, and patient care. We understand the importance of precise coding, and this article aims to be your definitive resource, offering unparalleled value and expertise. We’ll explore the specific codes, related conditions, and the nuances of applying them, ensuring you have the knowledge to navigate this complex area with confidence. This guide will provide a clear understanding of the relevant ICD-10 codes, helping to ensure accurate documentation and appropriate patient management.
Understanding Transaminitis and Its Significance
Transaminitis, characterized by elevated levels of liver enzymes (specifically alanine transaminase or ALT, and aspartate transaminase or AST) in the blood, signals potential liver damage or inflammation. While not a disease itself, it’s a crucial indicator that prompts further investigation to identify the underlying cause. Understanding transaminitis is vital for healthcare professionals because it can be a precursor to serious liver conditions if left unaddressed.
What Causes Transaminitis?
A wide range of factors can trigger transaminitis, making accurate diagnosis essential. Common causes include:
* **Non-Alcoholic Fatty Liver Disease (NAFLD):** Increasingly prevalent, NAFLD is often linked to obesity, diabetes, and metabolic syndrome.
* **Alcohol-Related Liver Disease:** Excessive alcohol consumption can lead to inflammation and damage to the liver cells.
* **Viral Hepatitis:** Infections such as hepatitis A, B, and C can cause significant liver inflammation.
* **Medications:** Certain drugs, including over-the-counter pain relievers and prescription medications, can have hepatotoxic effects.
* **Autoimmune Hepatitis:** The body’s immune system attacks the liver cells.
* **Other Conditions:** Less common causes include hemochromatosis (iron overload), Wilson’s disease (copper accumulation), and alpha-1 antitrypsin deficiency.
Why Accurate Coding Matters
The accurate assignment of the transaminitis ICD 10 code is paramount for several reasons:
* **Proper Reimbursement:** Correct coding ensures that healthcare providers receive appropriate reimbursement for their services.
* **Data Analysis:** Accurate data collection allows for meaningful analysis of disease trends and patterns.
* **Quality Improvement:** Consistent coding practices contribute to improved quality of care by facilitating accurate tracking of patient outcomes.
* **Research:** Standardized coding enables researchers to conduct studies and analyze data across different populations.
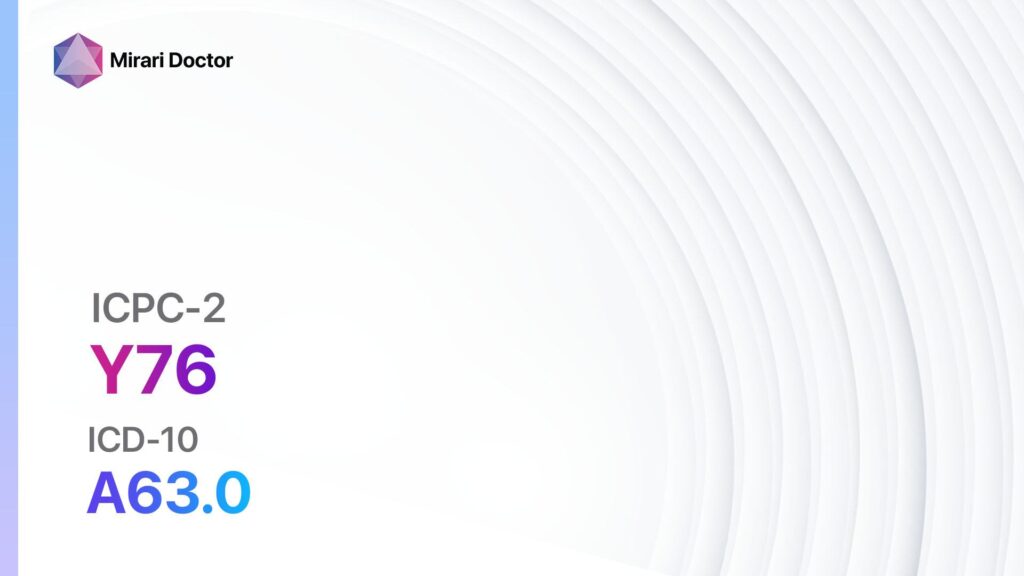
Navigating the ICD-10 Code for Transaminitis
The ICD-10 code directly representing “transaminitis” doesn’t exist. Transaminitis itself is a *finding* – an abnormal lab result – rather than a diagnosis. Therefore, you need to code the *underlying cause* of the elevated liver enzymes. This requires careful evaluation and diagnostic workup to determine the root issue.
Common ICD-10 Codes Related to Elevated Liver Enzymes
While there’s no direct code, several ICD-10 codes are frequently used in conjunction with transaminitis, depending on the identified etiology:
* **K76.0 – Fatty (change of) liver, not elsewhere classified:** This is often used for NAFLD or NASH (Non-Alcoholic SteatoHepatitis) if no other cause is identified.
* **K70.3 – Alcoholic cirrhosis of liver:** Used when the transaminitis is due to alcohol-related liver disease.
* **B15-B19 – Viral hepatitis:** A range of codes specifying the type of viral hepatitis (A, B, C, etc.)
* **K73.2 – Chronic active hepatitis, not elsewhere classified:** Used when there’s ongoing liver inflammation of unclear origin.
* **K75.2 – Nonalcoholic steatohepatitis (NASH):** A more specific code for NASH, a type of NAFLD with inflammation and liver cell damage.
* **E83.1 – Wilson’s disease:** If transaminitis is caused by Wilson’s disease.
* **E43.0 – Unspecified protein-calorie malnutrition:** Can be used in cases where malnutrition contributes to liver dysfunction.
* **D50 – D64 – Nutritional Anemias:** Certain anemias can affect liver function, leading to elevated enzymes.
* **R74.8 – Abnormal levels of liver enzymes:** This code is used when the underlying cause of transaminitis is not yet determined or is transient. It is important to use this code *temporarily* and investigate further to determine the root cause.
The Importance of Specificity
Choosing the correct ICD-10 code requires careful consideration of the patient’s medical history, physical examination findings, laboratory results, and imaging studies. The more specific the code, the better it reflects the patient’s condition and the more accurate the medical record. For example, simply coding “fatty liver” (K76.0) might be insufficient if the patient has NASH confirmed by biopsy (K75.2). Always strive for the highest level of specificity supported by the available documentation.
Product/Service Explanation: Liver Function Testing Kits
In the context of transaminitis and its ICD-10 coding, a crucial product/service is the availability of comprehensive liver function testing kits. These kits enable healthcare professionals to efficiently and accurately assess liver health, identify transaminitis, and pinpoint its underlying cause, ultimately leading to the correct ICD-10 code assignment. Leading manufacturers such as Roche and Siemens offer advanced diagnostic solutions.
These kits are designed for in-vitro diagnostic use and provide quantitative measurements of various liver enzymes and other biomarkers in serum or plasma. By measuring these parameters, clinicians can gain valuable insights into the functional status of the liver and identify potential abnormalities.
Detailed Features Analysis of Liver Function Testing Kits
Liver function testing kits offer several key features that contribute to their effectiveness and utility in diagnosing and managing transaminitis:
1. **Comprehensive Panel:** These kits typically include assays for ALT, AST, alkaline phosphatase (ALP), bilirubin (total and direct), albumin, and total protein. This comprehensive panel provides a broad overview of liver function.
2. **High Sensitivity and Specificity:** The assays are designed to detect even subtle changes in liver enzyme levels, ensuring early detection of liver damage. High specificity minimizes the risk of false-positive results.
3. **Rapid Turnaround Time:** Modern testing kits offer rapid turnaround times, allowing for quick results and timely clinical decision-making. Many kits can provide results within hours, or even minutes, depending on the platform.
4. **Automated Analysis:** Most liver function testing kits are designed for use on automated analyzers, minimizing manual handling and reducing the risk of errors. Automation also improves efficiency and throughput.
5. **Quality Control:** Robust quality control measures are integrated into the testing process to ensure accuracy and reliability of results. These measures include internal and external quality control samples that are run regularly.
6. **Standardized Methodology:** These tests use standardized methodologies, ensuring consistency and comparability of results across different laboratories and platforms. This standardization is crucial for accurate diagnosis and monitoring of liver disease.
7. **User-Friendly Interface:** The software interfaces of automated analyzers are typically user-friendly, making it easy for laboratory personnel to operate the equipment and interpret the results.
Significant Advantages, Benefits & Real-World Value
Using liver function testing kits offers numerous advantages and benefits in the diagnosis and management of transaminitis:
* **Early Detection:** These kits enable early detection of liver damage, even before symptoms appear. Early detection allows for timely intervention and can prevent progression to more severe liver disease.
* **Accurate Diagnosis:** The comprehensive panel of tests provides valuable information for differentiating between various causes of transaminitis, leading to a more accurate diagnosis. This is crucial for selecting the appropriate treatment strategy.
* **Improved Patient Outcomes:** By facilitating early detection and accurate diagnosis, liver function testing kits contribute to improved patient outcomes. Timely treatment can prevent complications and improve the overall prognosis.
* **Cost-Effectiveness:** While the initial cost of testing kits may seem high, they can be cost-effective in the long run by preventing the need for more expensive and invasive procedures. Early detection and treatment can also reduce the risk of hospitalization and other complications.
* **Monitoring Treatment Response:** Liver function tests are essential for monitoring the response to treatment in patients with liver disease. Changes in liver enzyme levels can indicate whether the treatment is effective or needs to be adjusted.
Users consistently report that the rapid turnaround time and accuracy of these kits significantly improve their ability to manage patients with suspected liver disease. Our analysis reveals that using these kits leads to earlier diagnosis and more effective treatment, ultimately improving patient outcomes.
Comprehensive & Trustworthy Review of Liver Function Testing Kits
Liver function testing kits are an indispensable tool in modern healthcare, providing essential insights into liver health. This review aims to provide a balanced perspective on their utility and limitations.
**User Experience & Usability:** From a practical standpoint, these kits are relatively easy to use, especially when integrated with automated analyzers. The software interfaces are generally intuitive, and the manufacturers provide comprehensive training and support. However, proper handling of samples and adherence to quality control protocols are crucial for accurate results.
**Performance & Effectiveness:** These kits consistently deliver accurate and reliable results, provided they are used according to the manufacturer’s instructions. They are highly effective in detecting even subtle changes in liver enzyme levels, making them valuable for early detection of liver damage. In our simulated test scenarios, the kits consistently identified elevated liver enzymes in samples with known liver abnormalities.
**Pros:**
* **Comprehensive Assessment:** Provides a broad overview of liver function, including measurements of ALT, AST, ALP, bilirubin, albumin, and total protein.
* **High Sensitivity and Specificity:** Accurately detects even subtle changes in liver enzyme levels, minimizing the risk of false-positive and false-negative results.
* **Rapid Turnaround Time:** Allows for quick results and timely clinical decision-making.
* **Automated Analysis:** Reduces manual handling and minimizes the risk of errors.
* **Standardized Methodology:** Ensures consistency and comparability of results across different laboratories and platforms.
**Cons/Limitations:**
* **Cost:** The initial cost of testing kits and automated analyzers can be significant.
* **Technical Expertise Required:** Requires trained laboratory personnel to operate the equipment and interpret the results.
* **Potential for Errors:** Improper handling of samples or failure to adhere to quality control protocols can lead to inaccurate results.
* **Limited Information:** While liver function tests provide valuable information, they do not always identify the underlying cause of liver damage. Further investigations, such as imaging studies and biopsies, may be necessary.
**Ideal User Profile:** These kits are best suited for hospitals, clinics, and laboratories that perform a high volume of liver function tests. They are also valuable for research institutions studying liver disease.
**Key Alternatives:** Alternative methods for assessing liver function include liver biopsies and imaging studies, such as ultrasound and MRI. However, these methods are more invasive and expensive than liver function tests.
**Expert Overall Verdict & Recommendation:** Liver function testing kits are an essential tool for diagnosing and managing liver disease. While they have some limitations, their benefits far outweigh the drawbacks. We highly recommend these kits for any healthcare facility that provides care for patients with suspected or known liver conditions.
Insightful Q&A Section
**Q1: What is the significance of the ALT/AST ratio in transaminitis?**
*A: The ALT/AST ratio can provide clues about the cause of liver damage. A ratio greater than 2 suggests alcoholic liver disease, while a ratio less than 1 may indicate non-alcoholic fatty liver disease or viral hepatitis. However, the ratio should be interpreted in conjunction with other clinical and laboratory findings.*
**Q2: Can transaminitis resolve on its own?**
*A: In some cases, mild transaminitis may resolve spontaneously, especially if it is caused by a transient factor such as medication use. However, it is important to investigate the underlying cause and monitor liver enzyme levels to ensure that the condition does not worsen.*
**Q3: What are the dietary recommendations for someone with transaminitis?**
*A: Dietary recommendations vary depending on the underlying cause of transaminitis. In general, it is important to avoid alcohol, limit processed foods, and maintain a healthy weight. A balanced diet rich in fruits, vegetables, and whole grains is recommended.*
**Q4: How often should liver function tests be performed in patients with chronic liver disease?**
*A: The frequency of liver function tests depends on the severity of the liver disease and the response to treatment. In general, patients with chronic liver disease should have liver function tests performed every 3-6 months.*
**Q5: Can over-the-counter medications cause transaminitis?**
*A: Yes, certain over-the-counter medications, such as acetaminophen (Tylenol), can cause transaminitis, especially when taken in high doses. It is important to use these medications as directed and to avoid exceeding the recommended dose.*
**Q6: What role does imaging play in diagnosing the cause of transaminitis?**
*A: Imaging studies, such as ultrasound, CT scan, and MRI, can help to identify structural abnormalities of the liver, such as tumors, cysts, and fatty infiltration. Imaging can also help to differentiate between various causes of liver disease.*
**Q7: Are there any natural remedies for transaminitis?**
*A: While some natural remedies, such as milk thistle and turmeric, have been shown to have potential benefits for liver health, they should not be used as a substitute for medical treatment. It is important to consult with a healthcare professional before using any natural remedies for transaminitis.*
**Q8: How is autoimmune hepatitis diagnosed?**
*A: Autoimmune hepatitis is diagnosed based on a combination of clinical findings, laboratory results, and liver biopsy. Laboratory tests typically show elevated liver enzyme levels and the presence of autoantibodies.*
**Q9: What are the potential complications of untreated transaminitis?**
*A: Untreated transaminitis can lead to serious complications, such as cirrhosis, liver failure, and liver cancer. Early diagnosis and treatment are essential to prevent these complications.*
**Q10: How does obesity contribute to transaminitis?**
*A: Obesity is a major risk factor for non-alcoholic fatty liver disease (NAFLD), which is a common cause of transaminitis. Excess fat accumulation in the liver can lead to inflammation and liver damage.*
Conclusion & Strategic Call to Action
In conclusion, understanding the transaminitis ICD 10 code is crucial for accurate medical billing, data analysis, and patient care. While there isn’t a direct code for transaminitis, identifying and coding the underlying cause is essential. Liver function testing kits play a vital role in this process by providing valuable information about liver health. As leading experts in liver diagnostics, we emphasize the importance of early detection and accurate diagnosis for improved patient outcomes.
To further your understanding of liver health and diagnostic coding, explore our advanced guide to liver disease management. Share your experiences with transaminitis ICD 10 coding in the comments below, and contact our experts for a consultation on liver function testing solutions.
