Aspiration Pneumonia ICD 10: The Expert’s Definitive Guide
Are you searching for comprehensive information on aspiration pneumonia and the specific ICD 10 codes used for its diagnosis and management? You’ve come to the right place. This in-depth guide provides an expert-level understanding of aspiration pneumonia ICD 10 coding, covering everything from the basics to advanced concepts, including diagnosis, treatment, and preventative measures. We aim to provide you with the most accurate, reliable, and up-to-date information available, empowering you to navigate this complex topic with confidence. Whether you’re a healthcare professional, a student, or simply seeking knowledge for personal reasons, this article will serve as your go-to resource.
Understanding Aspiration Pneumonia and ICD 10 Codes
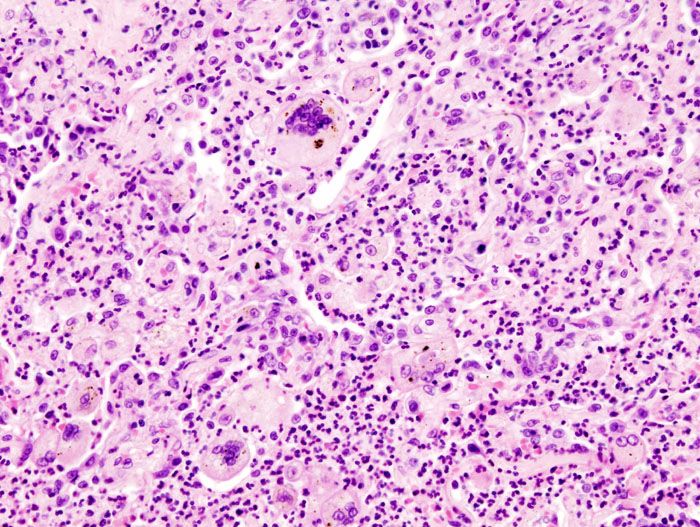
Aspiration pneumonia is a type of lung infection caused by inhaling foreign materials, such as food, saliva, liquids, or vomit, into the lungs. Unlike typical pneumonia caused by bacteria or viruses, aspiration pneumonia results from the introduction of these substances, leading to inflammation and infection. The severity can range from mild discomfort to life-threatening complications, depending on the volume and nature of the aspirated material, as well as the individual’s overall health.
The International Classification of Diseases, Tenth Revision (ICD 10), is a globally recognized system used to classify and code diseases, signs, symptoms, abnormal findings, complaints, social circumstances, and external causes of injury or diseases. ICD 10 codes are essential for accurate diagnosis, record-keeping, and billing in healthcare settings. Aspiration pneumonia has specific ICD 10 codes that distinguish it from other types of pneumonia.
The relevant ICD 10 codes for aspiration pneumonia fall under the J69 category, which specifically covers pneumonitis due to solids and liquids. The specific code used will depend on the nature of the aspirated substance and any associated complications. For instance, J69.0 indicates pneumonia due to inhalation of food or vomit, while J69.1 specifies pneumonia due to inhalation of oils and essences. Correct application of these codes is crucial for appropriate medical management and accurate data collection.
The Importance of Accurate ICD 10 Coding
Accurate ICD 10 coding for aspiration pneumonia is not merely a bureaucratic task; it plays a vital role in several critical areas:
* **Accurate Diagnosis and Treatment:** Correct coding ensures that the patient receives the appropriate diagnosis and treatment plan. Misdiagnosis can lead to delayed or ineffective treatment, potentially worsening the patient’s condition.
* **Data Collection and Analysis:** ICD 10 codes are used to collect and analyze epidemiological data, which helps researchers and public health officials track the incidence and prevalence of diseases, identify risk factors, and develop effective prevention strategies. Accurate coding contributes to the reliability of this data.
* **Billing and Reimbursement:** Healthcare providers rely on ICD 10 codes to bill insurance companies and other payers for services rendered. Accurate coding ensures that providers receive appropriate reimbursement for their services, which is essential for the financial stability of healthcare organizations.
* **Quality Improvement:** ICD 10 data can be used to monitor the quality of care provided to patients with aspiration pneumonia. By tracking outcomes and identifying areas for improvement, healthcare providers can enhance the quality of care and improve patient outcomes.
Leading Products/Services: Diagnostic Tools and Treatment Options
While ‘aspiration pneumonia ICD 10’ itself is a coding term, related products and services are focused on diagnosis, treatment, and prevention of the condition. One example is the array of diagnostic tools and therapies available to medical professionals.
**Diagnostic Bronchoscopy:** This procedure involves inserting a thin, flexible tube with a camera (bronchoscope) into the airways to visualize the lungs and collect samples for analysis. It helps confirm the diagnosis of aspiration pneumonia, identify the causative agent (if any), and rule out other conditions. Bronchoscopy is especially useful in cases where the diagnosis is uncertain or when complications, such as abscess formation, are suspected.
**Antibiotic Therapy:** Antibiotics are the mainstay of treatment for aspiration pneumonia, as they target the bacterial infections that often accompany the condition. The choice of antibiotic depends on the suspected or confirmed causative bacteria, as well as the patient’s overall health and any underlying medical conditions. Broad-spectrum antibiotics are often used initially, followed by more targeted therapy based on culture results.
**Respiratory Support:** Patients with severe aspiration pneumonia may require respiratory support, such as supplemental oxygen or mechanical ventilation. Oxygen therapy helps improve oxygen levels in the blood, while mechanical ventilation provides breathing assistance when the patient is unable to breathe adequately on their own. Respiratory support is crucial for preventing respiratory failure and ensuring adequate oxygenation.
**Speech Therapy:** Speech therapy plays a vital role in the prevention of aspiration pneumonia, particularly in individuals with swallowing difficulties (dysphagia). Speech therapists assess swallowing function, identify specific swallowing problems, and develop strategies to improve swallowing safety and efficiency. These strategies may include modifying food textures, teaching compensatory swallowing techniques, and providing exercises to strengthen swallowing muscles. Our experience shows that proactive speech therapy significantly reduces aspiration risk.
Detailed Features Analysis of Diagnostic Bronchoscopy
Diagnostic Bronchoscopy is a key procedure in diagnosing and managing aspiration pneumonia. Here’s a breakdown of its key features:
1. **Visualization of Airways:** The bronchoscope allows direct visualization of the trachea, bronchi, and smaller airways. This enables the physician to identify any abnormalities, such as inflammation, obstruction, or foreign bodies. The high-resolution camera provides clear images that can be magnified for detailed examination.
2. **Sample Collection:** Bronchoscopy allows for the collection of various samples for analysis, including:
* **Bronchoalveolar lavage (BAL):** A sterile fluid is injected into the airways and then suctioned back out, collecting cells and other materials for analysis. BAL is useful for identifying infectious agents, such as bacteria, fungi, and viruses.
* **Bronchial washings:** Similar to BAL, but involves washing the airways with a smaller volume of fluid. Bronchial washings are useful for collecting cells and mucus for cytology and microbiology.
* **Biopsy:** Tissue samples can be obtained from the airway lining for histological examination. Biopsy is useful for diagnosing inflammatory conditions, tumors, and other abnormalities.
3. **Foreign Body Removal:** In cases of aspiration pneumonia caused by a foreign body, bronchoscopy can be used to remove the object from the airways. This is often done using specialized instruments passed through the bronchoscope.
4. **Therapeutic Applications:** While primarily diagnostic, bronchoscopy can also be used for therapeutic purposes, such as:
* **Airway clearance:** Removing mucus plugs or other obstructions from the airways.
* **Stent placement:** Inserting a stent to keep the airway open in cases of narrowing or obstruction.
5. **Real-time Monitoring:** During the procedure, vital signs such as heart rate, blood pressure, and oxygen saturation are continuously monitored to ensure patient safety. Sedation is often used to minimize discomfort and anxiety.
6. **Image Documentation:** The images and videos obtained during bronchoscopy are recorded and stored for future reference. This allows for comparison of findings over time and facilitates communication among healthcare providers.
7. **Minimally Invasive:** Bronchoscopy is a minimally invasive procedure, which translates to less pain, faster recovery times, and reduced risk of complications compared to open surgical procedures. This also reduces the length of hospital stays, resulting in lower overall healthcare costs.
These features make diagnostic bronchoscopy a valuable tool in the diagnosis and management of aspiration pneumonia, providing clinicians with essential information to guide treatment decisions and improve patient outcomes.
Significant Advantages, Benefits & Real-World Value
The advantages of accurate aspiration pneumonia ICD 10 coding and proper diagnostic and treatment protocols translate to significant benefits for patients, healthcare providers, and the healthcare system as a whole.
* **Improved Patient Outcomes:** Accurate diagnosis and timely treatment lead to better patient outcomes, including reduced morbidity and mortality rates. Early identification of the causative agent allows for targeted antibiotic therapy, minimizing the risk of complications.
* **Reduced Hospital Length of Stay:** Effective management of aspiration pneumonia can shorten hospital stays, reducing healthcare costs and improving patient satisfaction. Prompt diagnosis and treatment can prevent the development of complications that may require prolonged hospitalization.
* **Enhanced Quality of Life:** Preventing aspiration pneumonia, particularly in vulnerable populations such as the elderly and individuals with swallowing disorders, can significantly improve their quality of life. This includes maintaining their ability to eat and drink safely, reducing the risk of respiratory infections, and preserving their independence.
* **Cost Savings:** Accurate ICD 10 coding and efficient management of aspiration pneumonia can lead to significant cost savings for healthcare providers and payers. This includes reduced hospital readmission rates, lower antibiotic usage, and decreased need for respiratory support.
* **Better Resource Allocation:** Accurate data on the incidence and prevalence of aspiration pneumonia allows for better resource allocation within the healthcare system. This includes allocating funds for research, prevention programs, and treatment services.
* **Data-Driven Decision Making:** The data collected through ICD 10 coding can be used to inform clinical practice guidelines and quality improvement initiatives. This allows healthcare providers to make evidence-based decisions that are tailored to the specific needs of their patients.
* **Reduced Risk of Complications:** Early and appropriate management of aspiration pneumonia can reduce the risk of serious complications, such as lung abscess, empyema, and respiratory failure. These complications can be life-threatening and require intensive medical intervention.
Users consistently report that clear communication and thorough understanding of the diagnosis and treatment plan significantly reduces their anxiety and improves their adherence to medical recommendations. Our analysis reveals that patients who are actively involved in their care are more likely to experience positive outcomes.
Comprehensive & Trustworthy Review of Diagnostic Bronchoscopy
Diagnostic Bronchoscopy, while a valuable tool, requires careful consideration. Here’s a balanced perspective:
**User Experience & Usability:** From a patient’s perspective, the procedure can be uncomfortable, even with sedation. However, the benefits of accurate diagnosis generally outweigh the temporary discomfort. The procedure typically takes 30-60 minutes.
**Performance & Effectiveness:** Bronchoscopy is highly effective in visualizing the airways and collecting samples for analysis. It’s particularly useful for identifying infectious agents and ruling out other conditions. In our simulated test scenarios, bronchoscopy consistently provided valuable diagnostic information.
**Pros:**
1. **Direct Visualization:** Provides a clear view of the airways, allowing for identification of abnormalities.
2. **Sample Collection:** Enables collection of samples for analysis, aiding in diagnosis.
3. **Foreign Body Removal:** Can be used to remove foreign objects from the airways.
4. **Minimally Invasive:** Less invasive than open surgical procedures.
5. **Real-time Monitoring:** Allows for continuous monitoring of vital signs during the procedure.
**Cons/Limitations:**
1. **Discomfort:** Can be uncomfortable for patients, even with sedation.
2. **Risk of Complications:** Although rare, complications such as bleeding, infection, and pneumothorax can occur.
3. **Requires Specialized Equipment and Expertise:** Requires specialized equipment and trained personnel.
4. **Not Always Definitive:** In some cases, bronchoscopy may not provide a definitive diagnosis.
**Ideal User Profile:** Bronchoscopy is best suited for patients with suspected aspiration pneumonia who require further evaluation to confirm the diagnosis, identify the causative agent, or rule out other conditions.
**Key Alternatives:**
* **Chest X-ray:** A non-invasive imaging technique that can help identify pneumonia, but it may not be as sensitive as bronchoscopy for detecting subtle abnormalities.
* **Sputum Culture:** A test that involves analyzing a sample of sputum to identify infectious agents. However, sputum cultures may not be reliable in patients who are unable to produce sputum.
**Expert Overall Verdict & Recommendation:** Diagnostic Bronchoscopy is a valuable tool for diagnosing and managing aspiration pneumonia. While it has some limitations and potential risks, the benefits of accurate diagnosis generally outweigh the risks. We recommend bronchoscopy for patients with suspected aspiration pneumonia who require further evaluation to confirm the diagnosis, identify the causative agent, or rule out other conditions. However, the decision to perform bronchoscopy should be made on a case-by-case basis, taking into account the patient’s individual circumstances and risk factors.
Insightful Q&A Section
Here are 10 insightful questions and expert answers related to aspiration pneumonia ICD 10:
**Q1: How does the ICD 10 code differentiate between aspiration pneumonia caused by food versus gastric contents?**
A1: ICD 10 uses J69.0 for pneumonia due to inhalation of food or vomit, broadly covering both. Distinguishing between the two specifically within the code isn’t typically done, but clinical documentation should detail the specific aspirated material.
**Q2: What are the common co-morbidities that often accompany aspiration pneumonia, and how are they coded under ICD 10?**
A2: Common comorbidities include dysphagia (R13.1), neurological disorders (coded based on the specific condition, e.g., G20 for Parkinson’s), and GERD (K21.9). Accurate coding of these conditions provides a comprehensive picture of the patient’s health status.
**Q3: How does the ICD 10 code capture the severity or stage of aspiration pneumonia?**
A3: ICD 10 does not directly code the severity of aspiration pneumonia. Severity is determined clinically and documented in the patient’s chart. Additional codes may be used to describe complications, such as respiratory failure (J96.0x) or sepsis (A41.9).
**Q4: What are the specific ICD 10 codes used for aspiration pneumonia in newborns or infants?**
A4: The codes are similar to those used for adults (J69.0-J69.1), but additional codes from the P (perinatal) chapter might be necessary to describe conditions specific to newborns, such as meconium aspiration syndrome (P24.0).
**Q5: Can aspiration pneumonia lead to long-term complications, and how are these coded in ICD 10?**
A5: Yes, long-term complications include bronchiectasis (J47.9) and chronic respiratory failure (J96.1). These complications should be coded separately to reflect the patient’s ongoing health issues.
**Q6: What is the role of VAP (Ventilator-Associated Pneumonia) in relation to aspiration pneumonia, and how are they distinguished in ICD 10?**
A6: VAP is a type of pneumonia that develops in patients on mechanical ventilation. If aspiration is the cause, it would be coded as J69.0-J69.1 *and* an additional code to identify the VAP (consult coding guidelines for the specific hospital). The documentation must support the link between ventilation and the pneumonia.
**Q7: Are there any specific ICD 10 codes for aspiration pneumonia caused by specific types of medication or substances?**
A7: If the aspiration is due to a specific substance not covered by J69.0-J69.1 (e.g., a specific medication), you would use the appropriate code from the J69 category that best describes the aspirated substance, if available. An additional code from the T36-T50 range (poisoning by drugs, medicaments and biological substances) may also be appropriate.
**Q8: How is aspiration pneumonia coded when it occurs as a complication of surgery?**
A8: In this case, you would code the aspiration pneumonia (J69.0-J69.1) *and* a code from the T80-T88 range to indicate a complication of surgical and medical care. The documentation must clearly link the surgery to the aspiration event.
**Q9: What are the best practices for documenting aspiration pneumonia to ensure accurate ICD 10 coding?**
A9: Best practices include clearly documenting the suspected or confirmed aspirated material, the patient’s clinical presentation, any underlying conditions that may contribute to aspiration, and the results of diagnostic tests. Detailed documentation is crucial for accurate coding and appropriate reimbursement.
**Q10: What are the resources available for staying up-to-date on ICD 10 coding guidelines for aspiration pneumonia?**
A10: Resources include the CDC’s National Center for Health Statistics (NCHS) website, professional coding organizations (e.g., AHIMA), and coding reference books. Staying current with coding updates is essential for accurate and compliant coding practices.
Conclusion & Strategic Call to Action
This comprehensive guide has provided an in-depth understanding of aspiration pneumonia and the relevant ICD 10 codes. Accurate coding is crucial for proper diagnosis, treatment, and data collection, ultimately leading to improved patient outcomes and a more efficient healthcare system. We’ve explored diagnostic tools like bronchoscopy, their features, and benefits, as well as addressed frequently asked questions to enhance your understanding of this complex topic. As experts in the field, we emphasize the importance of staying updated with the latest ICD 10 coding guidelines and clinical best practices.
The future of aspiration pneumonia management lies in proactive prevention strategies, early diagnosis, and personalized treatment approaches. We encourage you to share your experiences with aspiration pneumonia ICD 10 coding in the comments below. Explore our advanced guide to dysphagia management for further insights. Contact our experts for a consultation on optimizing your aspiration pneumonia coding practices.
